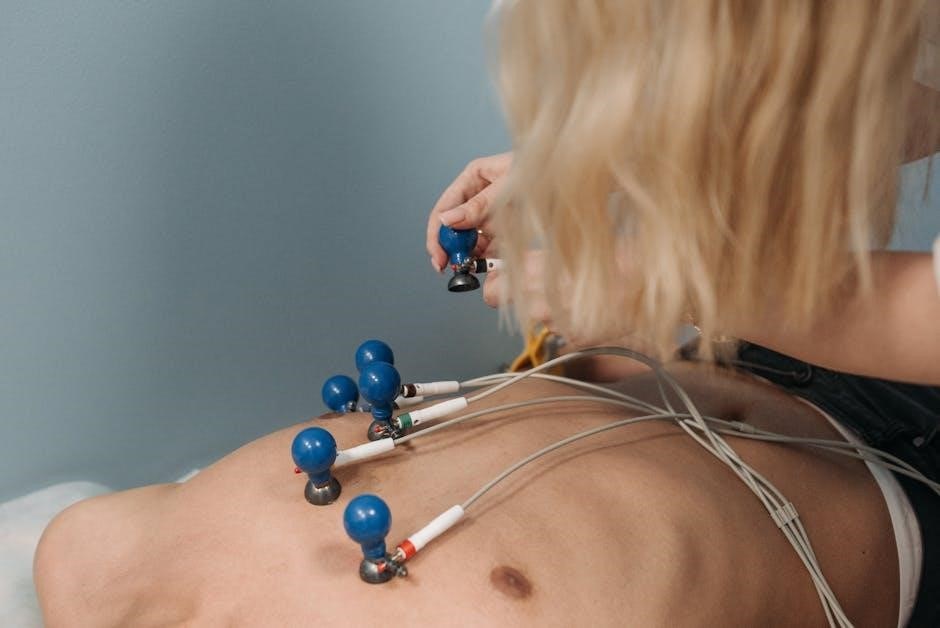
A 12-lead ECG is a diagnostic tool providing comprehensive cardiac electrical activity. Proper electrode placement ensures accurate readings, crucial for diagnosing heart conditions and avoiding misdiagnosis.
Overview of 12-Lead ECG
The 12-lead ECG is a fundamental diagnostic tool in cardiology, providing a comprehensive view of the heart’s electrical activity from multiple angles. It involves placing 10 electrodes on the body to record 12 different leads, offering insights into various cardiac conditions.
Each lead captures specific electrical signals, allowing healthcare professionals to identify patterns associated with ischemia, arrhythmias, or structural heart diseases. Proper electrode placement is critical to ensure accurate readings, as incorrect positioning can lead to misleading results. The 12-lead ECG is widely used in clinical settings, emergency rooms, and remote monitoring applications, making it an indispensable tool for both initial assessments and ongoing patient care. Its versatility and non-invasive nature have solidified its role as a cornerstone in cardiovascular diagnostics.
Importance of Proper Electrode Placement
Proper electrode placement is critical for obtaining accurate and reliable 12-lead ECG results. Incorrect placement can lead to misdiagnosis, as it may produce misleading or incomplete data.
Standardized positioning ensures that healthcare providers can accurately interpret electrical activity, identify patterns, and diagnose conditions such as ischemia or arrhythmias. Improper placement can result in false negatives or false positives, compromising patient care. Adhering to established protocols minimizes errors and ensures consistency across readings, making it essential for both routine and emergency situations. Proper placement also enhances the ability to monitor changes over time, aiding in effective treatment planning and patient outcomes. Thus, precise electrode positioning is a cornerstone of reliable ECG interpretation and quality patient care.

Basic Anatomy for ECG Placement
The heart’s electrical activity is captured via strategic electrode placement. Key anatomical landmarks include the fourth intercostal space, midclavicular line, and anterior axillary line for accurate readings.
Understanding the Heart’s Electrical Activity
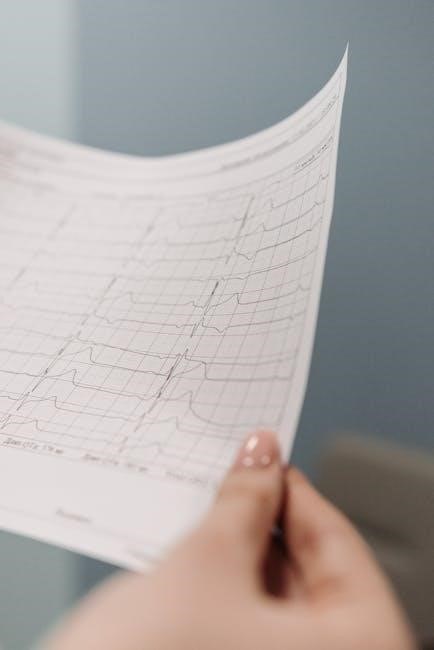
The heart’s electrical activity is captured through a 12-lead ECG, which records depolarization and repolarization of the atria and ventricles. Accurate electrode placement ensures precise readings, vital for diagnosing arrhythmias, ischemia, and other conditions. Misplacement can distort waveforms, leading to incorrect interpretations. The P wave represents atrial depolarization, while the QRS complex reflects ventricular depolarization. Correct placement aligns electrodes with the heart’s electrical axis, providing clear signals. This understanding is essential for interpreting ECGs accurately, making it a cornerstone in cardiovascular diagnostics. Proper placement avoids false diagnoses, ensuring reliable data for patient care.
Key Landmarks for Electrode Placement
Accurate electrode placement relies on identifying key anatomical landmarks. The manubrium of the sternum, at the angle of Louis, is the reference point for placing V1 and V2 electrodes. For V3 and V4, the mid-clavicular line serves as a guide. V1 is positioned to the right of the sternum, while V2 is placed to the left. The mid-clavicular line also helps locate V3, with V4 placed mid-way between V3 and V5. V5 and V6 are placed horizontally across the chest, aligned with the same horizontal level as V4. Limb electrodes are positioned on the distal ends of the arms and legs, avoiding joints. These landmarks ensure electrodes capture the heart’s electrical activity from multiple angles, providing a comprehensive 12-lead ECG tracing essential for accurate interpretation.
Step-by-Step Guide to 12-Lead ECG Placement
Ensure proper skin preparation. Place limb electrodes on arms and legs, referencing anatomical landmarks. Position precordial leads V1-V6 across the chest, following standardized placement guidelines. This ensures accurate ECG readings.
Limb Lead Placement (RA, LA, RL, LL)
Begin by placing the right arm (RA) electrode on the lateral aspect of the right arm, 1 cm above the wrist crease. The left arm (LA) electrode is positioned similarly on the left arm. For the right leg (RL) and left leg (LL) electrodes, place them 1 cm above the medial malleolus (ankle bone) on both legs. Ensure all electrodes are secured firmly to avoid movement. Proper alignment with anatomical landmarks is critical for accurate readings. Use a measuring tape to confirm distances if necessary. Clean and prepare the skin to ensure good adhesion and signal quality. Double-check electrode placement to prevent errors in ECG interpretation. Consistent placement across patients ensures reliable and comparable results.
Precordial Lead Placement (V1-V6)
Begin by placing V1 and V2 on the chest. Position V1 on the right side of the sternum, 4th intercostal space, and V2 on the left side of the sternum, same level. V3 is midway between V2 and V4. V4 is located at the mid-clavicular line, 5th intercostal space, aligned with the armpit. V5 is placed at the anterior axillary line, same horizontal level as V4, and V6 at the mid-axillary line. Ensure electrodes are securely attached and skin is clean for optimal signal. Adjust placements for body size; in larger patients, leads may be placed lower. Use rib landmarks to guide placement, ensuring accuracy for reliable ECG readings. Verify each lead’s position to prevent errors in interpretation.
Additional Tips for Accurate Placement
To ensure accurate 12-lead ECG placement, always use anatomical landmarks to guide electrode positioning. Double-check the placement of all leads before recording. For chest leads (V1-V6), ensure proper spacing and alignment with the mid-clavicular and axillary lines. In pediatric or obese patients, adjust lead placement as needed to accommodate body size. Avoid placing electrodes near scars or implants, as they may interfere with signal quality. Use the correct size of electrodes for the patient to ensure proper adhesion. Finally, maintain consistency in lead placement across patients to minimize variability in ECG interpretation. Always refer to a 12-lead ECG placement PDF guide for visual confirmation of correct positioning.

Common Mistakes in ECG Placement
Common mistakes in ECG placement include incorrect lead positioning, poor skin preparation, and inconsistent electrode placement, which can lead to inaccurate readings and misdiagnosis.
Incorrect Lead Positioning
Incorrect lead positioning is a frequent error in 12-lead ECG placement, often leading to inaccurate or misleading results. Even slight deviations from standardized positions can distort the ECG tracing, making interpretation challenging. Common mistakes include placing limb leads too high or too low on the extremities and mispositioning precordial leads, particularly V2 and V4, which are critical for detecting anterior and lateral wall abnormalities. Proper placement requires adherence to anatomical landmarks, such as the mid-clavicular line for V4 and the 4th intercostal space for V2. Inaccurate placement can mimic or obscure pathological conditions, emphasizing the importance of precision. Regular training and double-checking electrode positions are essential to minimize errors and ensure reliable ECG recordings.
Failure to Ensure Skin Preparation
Failure to ensure proper skin preparation is a common oversight in 12-lead ECG placement, potentially leading to poor signal quality. Skin should be clean, dry, and free of oils or lotions, as these can interfere with electrode adhesion and conductivity. Excessive hair or diaphoresis (sweating) can also compromise electrode contact, resulting in artifacts or low-quality tracings. Additionally, failing to remove jewelry or tight clothing near electrode sites can cause interference. Improper skin preparation may lead to inaccurate ECG readings, potentially mimicking or obscuring pathological conditions. Ensuring the skin is well-prepared is crucial for obtaining clear, reliable tracings and accurate diagnostic results. Proper preparation is a foundational step in the ECG process.
Ignoring Patient Positioning
Ignoring proper patient positioning during a 12-lead ECG can significantly impact the accuracy of the recording. Patients should ideally be placed in a supine position with their arms at their sides to minimize muscle artifact and ensure consistent electrode placement. Allowing the patient to move excessively or sit upright during the test can introduce artifacts, leading to inaccurate or uninterpretable tracings. Improper positioning may also cause baseline wander or electrical interference, obscuring important diagnostic details. Ensuring the patient remains still and in the correct position is essential for obtaining high-quality ECG recordings. Proper positioning is a critical step that directly affects the reliability of the electrocardiogram results.

Special Considerations
Special considerations in 12-lead ECG placement involve adapting techniques for pediatric, obese, and emergency patients. Proper adjustments ensure accurate readings in diverse clinical scenarios.
ECG Placement in Pediatric Patients
ECG placement in pediatric patients requires careful consideration of their smaller body size and varying proportions. Limb electrodes should be placed on the arms and legs, with the RL electrode often placed on the thigh in infants. Precordial leads (V1-V6) must be positioned according to the child’s chest size, avoiding the nipple line. Adjustments may be needed for premature infants or those with congenital heart defects. Using smaller electrodes and ensuring proper skin preparation is crucial to avoid discomfort and ensure signal clarity. Patient cooperation can be challenging, so a calm environment and age-appropriate communication are essential. Regularly updating skills in pediatric ECG placement is vital for accurate diagnostics in young patients;
ECG Placement in Obese Patients
ECG placement in obese patients presents unique challenges due to increased body mass, which can hinder electrode adhesion and signal quality. Proper technique is essential to ensure accurate readings. Use of larger electrodes or adhesive pads may be necessary to maintain contact. Skin preparation is critical; remove excess hair and ensure the skin is clean and dry. Electrode placement should follow standard anatomical landmarks, but deeper tissue may require adjustments in positioning. The precordial leads (V1-V6) should be placed directly over the chest, avoiding fatty tissue folds. Patient positioning, such as sitting upright, can improve breathing and signal clarity. Regular checks of electrode impedance are recommended to minimize artifacts. Training in handling obese patients enhances diagnostic accuracy and patient comfort.
ECG Placement in Emergency Situations
In emergency situations, rapid and accurate 12-lead ECG placement is critical for timely diagnosis and treatment. Ensure the patient is positioned comfortably, preferably in a supine position, to facilitate swift electrode application. Prioritize limb lead placement (RA, LA, RL, LL) first, as these are less affected by movement. Precordial leads (V1-V6) should be placed accurately, even under time constraints, to capture essential cardiac data. Use a systematic approach, such as the “torso circle” method, to quickly locate V1-V6 positions. Minimize patient movement during placement to avoid artifacts. If the patient is unstable, consider using a mnemonic or checklist to maintain focus. Once placed, quickly verify lead impedance and signal quality before finalizing the ECG recording. Promptly address any technical issues to ensure diagnostic accuracy in critical moments.
Advanced Techniques
Advanced techniques involve using mnemonics for precise electrode placement, optimizing ECG machine settings, and troubleshooting common issues to enhance accuracy and efficiency in 12-lead ECG placement.
Using Mnemonics for Lead Placement
Mnemonics are invaluable tools for mastering 12-lead ECG electrode placement. Techniques like “RA, LA, RL, LL, V1 to V6” help remember limb and chest lead positions. Mnemonics simplify complex steps, reducing errors and improving consistency. For example, “Chest leads from right to left” ensures proper V1-V6 placement. Mnemonics also aid in recalling anatomical landmarks, such as the V2 placement at the 4th intercostal space. Memory aids like “V3 halfway between V2 and V4” enhance accuracy. Mnemonics reduce cognitive load, allowing focus on patient comfort and precise placement. Regular practice with mnemonics improves speed and confidence, making them essential for both trainees and experienced professionals. Over time, mnemonics become second nature, ensuring reliable and efficient 12-lead ECG placement in clinical settings.
Optimizing ECG Machine Settings
Properly adjusting the ECG machine settings is critical for obtaining accurate and interpretable tracings. Begin by ensuring the machine is calibrated to the standard settings: 10mm/mV for amplitude and 25mm/sec for paper speed. Select the appropriate filter settings, typically 0.05Hz to 150Hz, to minimize noise while preserving diagnostic information. Adjust the gain to ensure the ECG tracing is clear and within the standard range. Check electrode impedance to confirm low resistance, as high impedance can distort signals. Regularly maintain and update the ECG machine to ensure optimal performance. Additionally, verify that the machine is set to record all 12 leads simultaneously. Proper machine settings enhance trace quality, reduce artifacts, and ensure reliable diagnostic results. Regular checks and adjustments are essential for consistent accuracy.
Troubleshooting Common Issues

Identifying and resolving issues during 12-lead ECG placement is crucial for accurate results. Common problems include artifacts from muscle tremors, electrical interference, or poorly prepared skin. Check for loose or misplaced electrodes, as these can cause signal drift or poor trace quality. Ensure all leads are securely attached and verify proper connection to the machine. If interference persists, consider using a higher-quality ECG machine or relocating the patient away from electrical sources. Address patient-related issues, such as movement or respiratory artifacts, by encouraging relaxation and deep breathing. Regularly inspect electrodes and cables for damage or wear. Correcting these issues promptly ensures reliable and interpretable ECG tracings, improving diagnostic accuracy and patient care.
Learning Resources
Access comprehensive guides, online courses, and practice worksheets to master 12-lead ECG placement. These resources are ideal for both beginners and experienced professionals, ensuring hands-on practice and mastery.
Recommended PDF Guides
Multiple high-quality PDF guides are available online, offering detailed instructions on 12-lead ECG placement. The American Heart Association (AHA) and ECRI provide comprehensive resources, including step-by-step diagrams and troubleshooting tips. These guides often include anatomical illustrations, electrode placement charts, and case studies to enhance learning. Many PDFs are designed for healthcare professionals, with a focus on standardization and accuracy. They also cover common pitfalls, such as incorrect lead positioning and skin preparation errors. Some guides are tailored for specific populations, like pediatric or obese patients. These resources are invaluable for both students and experienced practitioners, serving as quick references or in-depth study materials. Downloading these PDFs ensures access to reliable, evidence-based information anytime.
Video Tutorials and Demonstrations
Video tutorials are an excellent resource for mastering 12-lead ECG placement. Platforms like YouTube and Vimeo offer step-by-step demonstrations by healthcare professionals. These videos provide visual guidance on electrode positioning, ensuring accuracy and consistency. Many tutorials include real-life examples, highlighting common mistakes and how to avoid them. Some videos also cover special scenarios, such as pediatric or obese patients. Interactive simulations and 3D animations further enhance understanding. Institutions like the AHA and medical schools often share high-quality instructional videos. These tools are particularly useful for hands-on learners, allowing them to observe proper techniques and practice alongside the demonstrations. They complement written guides, offering a dynamic learning experience that improves proficiency in ECG placement.
Interactive Tools and Apps

Interactive tools and apps are invaluable for mastering 12-lead ECG placement. Applications like ECG Simulator and HeartECG offer virtual practice environments where users can explore electrode positioning through simulations. These tools often feature quizzes and case studies to reinforce learning. Many apps include 3D models of the heart, allowing users to visualize electrode placement from various angles; Furthermore, some platforms provide real-time feedback, highlighting errors in placement and suggesting corrections. These resources are particularly beneficial for visual and kinesthetic learners, as they allow hands-on practice without the need for physical equipment. Regular use of these tools can significantly improve proficiency in ECG placement, ensuring accurate and reliable results in clinical settings. They also serve as convenient references for healthcare professionals looking to refresh their skills, aiding in continuous education and professional improvement.
Tricks of the Trade
Experienced professionals use mnemonics like “PLVx” for precordial leads and ensure consistent landmarks for accuracy, reducing errors in 12-lead ECG placement.
Expert Tips for Consistent Placement
Experienced technicians emphasize the importance of standardizing the process to ensure accuracy. Always use anatomical landmarks like the clavicle and nipple line for precise electrode positioning. Double-check electrode quality and skin preparation to minimize artifacts. For consistency, mark electrode sites with a pen if repositioning is needed. Use a systematic approach, starting with limb leads and progressing to precordial leads. Ensure the patient remains still and breathing normally during placement. Documenting electrode positions can help maintain accountability. Regular practice and feedback from senior technicians can refine skills. Following these expert tips ensures high-quality, reproducible 12-lead ECGs, critical for accurate cardiac assessments and patient care.
Time-Saving Strategies
To streamline the 12-lead ECG process, prioritize preparation and organization. Pre-measure and label electrodes before application to save time. Use mnemonic devices to remember lead placements quickly and efficiently. Batch tasks by placing all limb electrodes first, followed by precordial leads. Standardize your setup by ensuring the ECG machine is prepped and ready. Utilize a checklist to verify each step swiftly. Minimize repositioning by marking electrode sites if adjustments are needed. Practice consistent workflows to reduce delays. These strategies not only save time but also enhance accuracy, allowing for faster patient throughput without compromising quality. Efficiency is key in busy clinical settings.
Ensuring Patient Comfort
Ensuring patient comfort during 12-lead ECG placement is crucial for accurate results and a positive experience. Create a calm environment by explaining the procedure clearly. Allow patients to lie still in a comfortable position, as movement can interfere with readings. Keep the room at a comfortable temperature to prevent shivering. Use hypoallergenic electrodes if the patient has sensitive skin. Avoid unnecessary exposure by covering areas not requiring electrode placement. Minimize disruptions by organizing electrodes and wires neatly. Be mindful of cultural sensitivities when exposing skin. Ensure the patient is relaxed, as tension can affect heart activity. Proper preparation and empathy significantly enhance patient comfort, leading to better cooperation and outcomes.
Mastering 12-lead ECG placement ensures accurate diagnostic results. Proper electrode positioning and patient preparation are key to reliable readings. Continuous learning enhances proficiency in this essential skill.
Final Checklist for 12-Lead ECG Placement
- Ensure all electrodes are correctly positioned on the limbs and chest.
- Verify proper skin preparation by cleaning and drying the areas.
- Check electrode adhesion and secure any loose connections.
- Confirm the ECG machine is set to the correct calibration and filter settings.
- Position the patient in the supine position with arms relaxed.
- Double-check lead labels (RA, LA, RL, LL, V1-V6) for accuracy.
- Monitor for electrical interference and ensure a quiet environment.
- Document the patient’s name, date, and time on the ECG tracing.
- Dispose of used electrodes properly after the procedure.
This checklist ensures accurate and reliable 12-lead ECG results, minimizing errors and enhancing diagnostic confidence.
Continuous Learning and Improvement
Continuous learning is essential for mastering 12-lead ECG placement. Regular practice and review of electrode placement techniques ensure consistency and accuracy. Staying updated with the latest guidelines and advancements in ECG technology is crucial. Engage in ongoing education through workshops, webinars, and certified training programs. Utilize online resources, such as PDF guides and video tutorials, to reinforce best practices. Seek feedback from experienced professionals to identify and correct common errors. Reflect on challenging cases to improve problem-solving skills. By dedicating time to learning and refinement, healthcare professionals can enhance their proficiency in 12-lead ECG placement, ultimately improving patient care and diagnostic outcomes.




About the author